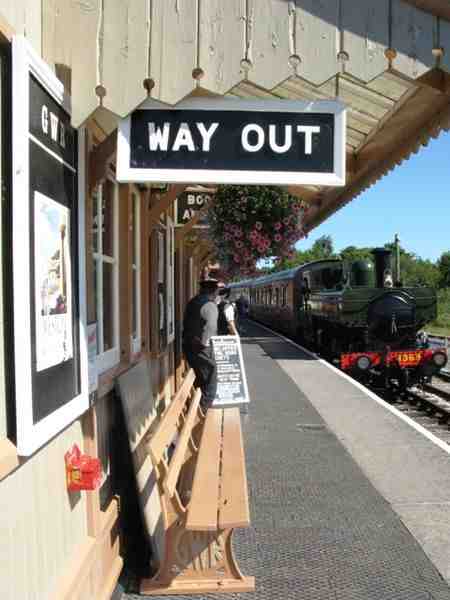
 As you enter the Devon town of Totnes you will greeted with the ‘Welcome to Totnes’ sign under which an insightful wag has sprayed, ‘Twinned with Narnia’.
As you enter the Devon town of Totnes you will greeted with the ‘Welcome to Totnes’ sign under which an insightful wag has sprayed, ‘Twinned with Narnia’.
The town has a reputation for embracing all things alternative. It has countless alternative medicine practitioners. The Society of Homeopaths have their ‘education’ centre here. There is the Schumacher College that offers an MSc in ‘Holistic Science’. It has a Steiner School. Only two-thirds of children get vaccinated against MMR compared with over 90% in neighbouring towns.
As such, it was a delight to be invited to sit on a panel for a debate at Dartington Hall entitled, “Does Integrated Medicine Make Sense?” The debate was scheduled after Totnes became the centre of a controversy where Trading Standards were asking a local doctor not to hold a conference on treating cancer with alternative medicine as it might fall foul of the law. Was this an attack on free speech, or an attempt not to allow quacks to exploit people with cancer?
The debate was hosted by David Parsley of Totnes FM who did a sterling job of putting Dr Hopwood on the spot over his cancer conference. On the panel with me were: Dr Sarah Wollaston, the local MP for Narnia, who was calm and measured in the defence of evidence based medicine; Becky Simpson, who is currently living with cancer and was passionate and enthusiastic about the merits of diet, fitness, acupuncture and sodium bicarbonate alongside her conventional treatment; and Simon Mills, a herbalist who has been working with the College of Medicine.
The audience drew in people of all stances on these issues with many people from The Disputables, a debating group from Plymouth who helped organise the debate, but about two-thirds were from local communities and included homeopaths, alt-med practitioners, conspiracy theorists and Anthroposophists (I was told I could spot these from the cold, dead eyes that would stare back at me.)
Dr Stephen Hopwood, who kicked off the controversy with his conference, was in attendance with supporters. His only question was unfortunately rather lame (“Why has modern medicine given us so little to boost the immune system?”. ) Other questions enquired as to what we could do to stop the supermarkets from deliberately adding poisons to our food, and what did we think of advances in psychoneuroimmunology and how that would effect the epistemology of holistic mind/body medicine, or something, from a NPL practitioner and registered ethno-medicine practitioner with a correspondence D.Sc from the Open International University for Alternative Medicine in India.
This form of debate is often entertaining, but it is difficult to develop any length of coherent argument as you are reduced to short answers to disparate and unconnected questions from the audience. The central question of does “Integrated Medicine Make Sense?” was somewhat hampered by all panellists, at least in principle, agreeing that mainstream medicine was very important that good evidence was also vital. Members of the audience will have had divergent views.
So, I shall try to bring up a few issues raised by the debate in forthcoming blog posts. In the meantime, here is my introductory speech that I offered at the start. After which I will attempt to answer the closing question of the conference,
The idea that patients should experience an integrated approach to their health care is not controversial. We should expect that the various social, physical, mental – and dare I say, spiritual, elements of health be blended in a way that is efficient and seamless, and that respects a patient’s individual needs and autonomy.
This may not be controversial. And we may all agree a patient’s unique needs and preferences should be at the centre of health provision.
But what is controversial is the how the term ‘Integrated Medicine’ has been misappropriated by certain factions. It has been hijacked by those that want to raise the profile of pseudoscientific and superstitious forms of therapy. It is merely the latest way dubious treatments are being branded and promoted. What was once simple quackery became alternative medicine. It then shifted to ‘complementary’, and, has now moved to ‘integrated medicine’. It hijacks the term by insisting that such treatments should be available, often publicly funded, as part of the respect for patient’s choices and their own individuality.
But such treatments, either unproven and irrational, or disproven and discredited, do not add to patient choice. In fact, they distort the very meaning of informed choice. They undermine the basic concepts of how patients should understand the balance of risks and benefits.
I believe it is a central strategy of those promoting Integrated Medicine to undermine the most important question in medicine: how we know what works and what does not work. And how we know what is safe and what carries risks. Getting these questions wrong means that people will get hurt and will die.
There are calls to be more broadminded about evidence, claims that trials cannot work for a particular individualised treatment, and appeals to accept anecdotes over data. Personal interpretations of experiences are supposed to trump more objective reviews of the available evidence base. Implausible science is brushed aside. Pseudoscience is embraced. In deliberately confusing what constitutes reliable evidence and robust science, IM actual removes the ability for people to make genuinely informed choices. It privileges the practitioners beliefs over a patients right to understand the evidence.
But of course, many people report positive experience with such treatments. The veneer of care that is layered on the pseudoscience can make a person feel that their concerns and needs are being met. But there is a deliberate conflation of the concepts of care with treatment. If we want to improve compassionate care whilst people undergo treatment, the answer is not to delegate that aspect to those with often bizarre and false beliefs, but to improve mainstream care.
And of course there are risks. Many practitioners may present themselves as complementary but actual hold deeply antagonistic views towards mainstream medicine. Claims will be made without good evidence. Attacks on the integrity of doctors are routine. False beliefs about vaccination, diet, medicines and risks are imparted. Wedges are driven between patient and doctor. And the risks of the alternative treatment are denied or downplayed. Very often, the risks are completely unknown.
Integrated Medicine does not make sense. It tries to integrate science with nonsense, and evidence with superstitious belief. It continues to exist because there is no culture of critical self-appraisal within the community of practitioners. No mechanism for ever excluding error and improving knowledge. All claims are accepted as part of the mantra of individuality and choice. And when all claims are accepted uncritically, genuine informed choice and autonomy are impossible. Integrated care can only be delivered by evidence. The alternative is to abandon the patient on the alter of dogma, and that is an unforgivable disservice.
The conference closed with a question from a member of the audience about how mainstream and alternative medicines can be reconciled? How can they work together?
I must admit I do not know. At the heart of the problem is a respect for evidence and science. It is not clear how practitioners can work together when one believes that evidence should be used to inform treatment options and the other believes that whatever evidence is available should be used to support prior beliefs.
The problem with alternative medicine is not that they are unscrupulous charlatans rather that you are debating people about their very definition of themselves. When you have defined yourself as a homeopath, acupuncturist or chiropractor, no amount of contrary evidence will ever shift your core beliefs about yourself. Mainstream medicine tends to be organised around specialities not tied to specific treatments (on the whole). If evidence suggests a certain drug may not be effective, but that exercise might be, then you do not have to redefine who you are in order to change your practice. Your GP is not a Statinist, but someone who will be grappling with the changing evidence for the effectiveness and safety of statins, albeit imperfectly, no doubt.
This is not possible in alternative medicine. For that reason, genuine critical appraisal of techniques never occurs. Beliefs in effectiveness are axiomatic, not derived from evidence. How can modern medicine co-exist with such worldviews without misleading and confusing patients?
I do not know. It is true that ethical forms of genuinely complementary medicine could exist and maybe do exist in pockets. But I see little evidence of that. My next blog post will discuss one of the supporters of ‘Integrated Medicine’ in cancer care that was brought up at the conference. It will not be pretty reading.
TQ9er: a mark that is alleged to have appeared on some doctors’ notes when presented with a denizen of Totnes who may have unconventional beliefs about health and medicine. Derived from the postcode of the town.
Very nice blog post.
One might as well ask how the geocentric and heliocentric planetary systems can be reconciled. One is true and the other patently false, and no amount of insisting, hand-wringing or lexical gymnastics will make the geocentric planetary system reality.
It is, in my opinion, a matter of reality versus alternative reality.
Do tell, please. Which system is patently false, and which of its predictions contradicts observations?
You’ve got the burden of proof backwards there Terrence. When you make an efficacy claim for a particular treatment, it behooves you to provide the evidence that supports your claim.
Oh, I was commenting only on the astronomical theories, and even there my issue is only with pv’s claim that the geocentric theory is “patently false”.
The advantages of the heliocentric theory are many. Notably, the geocentric theory can accommodate additional epicycles, and this reduces the falsifiability of the theory. The heliocentric theory, by contrast, economically wrings much out of the inverse-square property of gravity. But still, “patently false”? (For the sake of a good argument, readers will charitably overlook the “crystalline spheres” bit, won’t you?)
Which are better, proven medical techniques, or unproven ones? Is it is provably better to offer a mix of proven and unproven techniques? Or is this just wishful thinking?
Tough question…
Would you like your salad mixed with garden refuse, just in case it tastes better?
That isn’t really a remotely tough question. Not least because in this case, calling the treatments unproven is very misleading: the vast majority have been proven to be ineffective or in some cases actively harmful. (e.g. reports of chiropractic leading to strokes by way of dissecting carotid aneurysms.)
Also the way you ask suggests that there is no way to find out; we can design tests to answer all of your questions. Many such tests have already been done. (Although to test the kind of “unproven” treatments that I imagine you mean against proven treatments would most likely be grossly unethical. E.g. a chemotherapy vs aromatherapy trial for cancer patients would rightly never be allowed.)
As always I enjoyed your post, Andy. May I suggest some more euphemisms used by quacks in the last few decennia? In a more or less chronologic sequence we saw:
Natural medicine
Paranormal medicine
Alternative medicine (1974)
Additive treatments
Integral medicine
Hoilistic medicine
Pluriform medicine
Complementary medicine
Integrated medicine
CAM
Integrative medicine.
More can be expected in the near future!
One question regarding your speech: what did you mean with:’Implausible science is brushed aside.’?
As highlighted above, the final question is key, because it demonstrates the core fallacy. How should alternative and mainstream be reconciled? They shouldn’t. It is that simple. Either something provably works, or it is alternative.
Surely something that doesn’t work isn’t an alternative.
An alternative to medicine rather than “alternative medicine”, perhaps.
Yes!
“An alternative to medicine rather than “alternative medicine”, perhaps”
From this point on I shall refer to it as such.
Alternative TO medicine.
Very well said Andy. I would love to read a transcript of this meeting.
I believe a recording may be available soon.
I was sad not to be there. My own post-code is TQ6, in which the numeral “9” is upside down,(or the correct way up)as you might expect!
As a Consultant Pedant I do need to mention that Dr. Sarah’s name is Wollaston. Only one “o” after W.
Thanks. Corrected. Had the name Woollams on the brain – next blog post.
Andy Lewis said:
I hope you get better soon.
Me too on the get well soon front.
Ainsworths probably have a 30C “Name Woollams” nosode to help your recovery.
Interesting question you got on ‘boosting the immune response’. There is no strategy in learned medicine to boost normal general immune responses above normal, leaving specific vaccines aside. It is however one of the false continuous claims made for alternative strategies. No measurements of course are made.
I read somewhere that you don’t really want a continuously boosted immune system as autoimmune diseases may result. Don’t know if there is anything to that, but it seems right.
I made a similar point at the gig. Yes, language is a bit difficult here as terms like ‘boost’ are not defined. But, yes, the immune system can indeed ‘go on the rampage’ against the self.
I think, from reading woo posts, that the question “Why has modern medicine given us so little to boost the immune system?” has a lot of ideology behind it.
Woos seem to conflate the immune system with some “vital force”. If you defocus your mind for a moment it kind of makes sense. The immune system permeates the whole body and if it fails, you die. It also fits well with holistic mind/body confusions; compare autoimmune disease with the idea of a guilty conscience “gnawing away” at you or falling ill with capitulating to some malign authority.
I suspect Dr Hopwood thinks there is an answer to his question that runs something like this:
Rational materialistic modern medicine has not appreciated the essentially mystical character of the immune system and has therefore been unable to understand what is required to boost it.
As such it has the same significance to health woos as the supposed impossibility of explaining how an eye might have evolved does for the creationist. The skeptic isn’t supposed to have an answer and the failure to answer is taken as proof the woo world view is correct.
It’s a good question. I’ve thought about why Hopwood would ask such a banal question at an an event that was in many ways kicked off by his actions.
Somehow, he must think this is a deeply fundamental question that exposes his critics’ stances.
Who knows?
Modern medicine can boost the immune system in many ways.
Cancer patients and transplant patients are given drugs to boost white cell count, as their treatments damage bone marrow, and these drugs compensate somewhat for that damage. For example my mother received Sargramostim (or similar drug) as part of her transplant treatment, and her white cell count recovered quickly.
Many commonly prescribed drugs are about mitigating the damage the immune response does. Think non-steroidal anti-inflammatories. Medicine (at least for cancers and infectious diseases) is mostly concerned with issues where the normal immune response is either insufficient (i.e. the person didn’t just get better, or is getting better too slowly), or problematic (autoimmune, or just painful).
So in essence the answer to the question is, because that isn’t a very useful method of treating disease.
Cancer patients may receive advice on nutrition and similar to ensure their immune response is not compromised by silly behaviour, but at the end of the day the immune response only goes so far, and in many cases evolution has already fine tuned that response (because not surviving disease is a strong selective pressure), and in many cases evolution will favour surviving with unnecessary damage from the immune response, over not surviving, since the dead tend not to reproduce.
I laughed at the notion of doctors marking patients notes with “TQ9er” as an indication of general stupidity and an inclination toward quackery and mumbo-jumbo.
When I was a mere yoof back in the late 60s doctors used to get (and presumably still do) loads of patients who were “out of sorts”, “suffering from a general malaise”, “whose get up and go had got up and gone”, “not feeling myself”, “feel tired and listless” – ad nauseum (but without any actual nausea).
In many respects these were the general conditions that Valium and Librium were invented for – as immortalised in the Stones “Mothers Little Helper” – to help her on her way, get her through her busy day.
Doctors would mark patients notes with “TATT Syndrome” as most of the patients were “Tired All The Time”.
If patients did not actually need Valium/Librium doctors would prescribe SFA as a proven cure for TATT syndrome. SFA was “sweet fanny adams” and was a sugar placebo. Homeostupidity didn’t seem to be around much then but I suppose they could have prescribed that – although I suppose it is the same difference in that sugar pills are sugar pills.
Obviously no doctor would be that unethical nowadays (apart from the two who recently recommended acupuncture to me – and got told where to go in no uncertain terms).
Maybe TQ9 should be redesignated Tattnes.
Brilliant! That’s the best yet.
I’m plairgarising it immediately.
And to think I am Honorary Secretary for the South Devon Division of the BMA which includes… Tattnes!
I’ll be using it at this years Annual Conference!
Richard
Well well Dr Rawlins, i think you perhaps have just dishonoured your honorary title of your regional B.M.A. What is there ‘line’ regarding derogatory appellations for patients who seek the wider view on health, and illness prevention and cure?. You have the only answers do you?
Incidentally, when you’re ‘plairgarising’, be sure to plagiarise the spelling correctly!!.
In the meantime i have just viewed more inspiring evidence of Gerson therapy being acknowledged for Cancer treatment, namely in Japan where mainstream Medicine there is embracing it. Cancer out the way it came in being my take on addressing a Cancer diagnosis. Perhaps Dr, the N.H.S attitude is why the U.K straggles behind in Cancer care particularly. Incidentally, do you engage in Medical neglect by Prescribing Statins?. I would be interested to know.
Meantime, I shall promote Gerson Therapy as a Cancer treatment with the complete intention of CURE!!!. You can stick your Cancer Act 1939 down where thousands of Cancer patients have been consigned to death through ignorance of alternatives, ignorance perpetuated by a highly profitable cut, poison, or burn prescription. We are overdue for a revolution in Health, as with many a BIG CORPORATION attack on truth and evidence… [vis a vis G.M trial at Rothamsted Research under guise of state funding]
[email protected]
Nigel: Could you provide a link to the evidence that Gerson therapy, or indeed any “alternative” treatment, has any efficacy in the management of cancer? By evidence, I mean decent quality, published in peer-reviewed scientific journals. Do not link to crappy testimonials as that will likely be treated with the contempt it deserves.
By the way, if you are going to make snarky remarks about spelling, it helps if you can avoid multiple spelling and grammatical errors yourself.
Nigel: Could you provide a link to the evidence that Gerson therapy, or indeed any “alternative” treatment, has any efficacy in the management of cancer? By evidence, I mean decent quality, published in peer-reviewed scientific journals. Do not link to crappy testimonials as that will likely be treated with the contempt it deserves.
By the way, if you are going to make snarky remarks about spelling, it helps if you can avoid multiple spelling and grammatical errors yourself.
Please list the ‘errors’ i have purportedly made. I would appreciate the education. I cannot spot any myself.
Returning to the subject, please refer to my response to Liz under the ‘Burzynski comes to the U.K’ link..
Regards….
http://en.wikipedia.org/wiki/Dunning%E2%80%93Kruger_effect
Nigel
You are an example of Muphry’s Law as well as the DK effect.
Just for starters when you use i it is usually capitalised as I.
Answer: I do not prescribe statins. Not my field. I do recognise 5% of patients will have myopathy. It is a matter of risk and benefit. Each patient has to make their own choice.
Orthodox doctors are desperate to find help in the management of cancers. If there was plausible evidence for Gerson therapy being of help, of course othodox practitioners would use it. Why on earth do you imagine they would not? Should be a Nobel prize in there for someone.
Yes, commercial organisations will try to take every commercial advantage. That is precisely why good doctors demand proper scientific evidence being produced for ANY healthcare claim. We really are on your side you know. Please do not feel paranoid or ascribe un-worthy motives to doctors in general. Big Charma (Complementary Health and Remedy Medicine) has the same faults and problems as Big Pharma.
If you are content using alternatives to rational scientific based medicine, that’s your choice, but please try to understand why so many orthodox practitioners refer to such interests as “woo”. Can you really blame us?
Best wishes.
OK then Dr.R.R, payback time.
If you are plagiarising my TATTnes then I am immediately plagiarising your Big Charma.
Just a pity that it sounds rather pleasant.
As a suggestion you might want to leave off the C and make it homophonous with what it actually does (using as my reference source: http://www.whatstheharm.com).
Damn.
I forgot to use the (c) sign – not least because it does not appear on a sodding iSad keyboard.
The doctor who told me that was yet another of my Irish uncles (or somesuch). The Vatican has a lot to answer for.
His surgery was the downstairs of an old Victorian terraced house in Isleworth. The front room was the surgery and the back room was the waiting room. Neither room had been decorated since Victoria was Empress of India. There was a downstairs toilet but you had to be really desperate or suffering from amoebic dysentery to even go near it.
I think he was running biological warfare experiments behind the peeling wallpaper. Perhaps he had a sideline going with the Pentagon and shipped his bacteriological output to Vietnam for field trials (this was 1969).
If you went to see him he always had a fag on the go. Nor was he a stranger to a bottle of Flowers.
The waiting room was a “turn up and hang about until your turn comes or you die – whichever comes first” one. Everybody in it smoked like chimneys. You could get lung cancer just waiting to have a boil seen to.
Every patient looked very shifty. This was partly because they were coveting their position in the queue, partly because they only really wanted a sick note to skive off work and partly because there was a real danger of running out of fags before your turn came up.
My current health centre looks like something out of Startrek by comparison.
My daughters do not believe me when I tell them this.
John your web site is excellent!
I only hope the Homeopaths do not see yout heart shaped drop of water!
Nigel:
Sigh…I knew I’d regret it but I looked at your response as suggested. You referred to the deranged ramblings of Liz with the words, “Sanity speaks.” You then followed with a barely less incoherent screed. No links to anything that might be construed by a rational individual as evidence. You are clearly beyond reason.
Regarding your spelling and grammar issues, I simply can’t be bothered.
Churlish not to mention any of Simon Mills’ contribution on that evening – intelligent, informed, diplomatic – I think we are seeing the transition from ridicule to violent opposition and we know what comes next 🙂
I do intend to write more about several aspects of the debate, including Simon’s stance. In the meantime, hope to see you at Plymouth Skeptics in the Pub in a week or do.