There are a number of differences between the practices of medicine and the pseudo-medicines, such as homeopathy, acupuncture and herbalism.
One of the most important is the practitioners attitude to a treatment’s safety and efficacy. Within the world of alternative medicine, efficacy and safety is axiomatic. That is, practitioners believe in the power of their treatments because it is doctrinal and not as a result of robust empirical and theoretical results.
In medicine, a new treatment, whether that be surgical, pharmaceutical or other, may start off as an idea: an insight, hypothesis or hunch. Evidence is gathered to see if that idea is correct or not. The plausibility of the treatment needs to be understood, albeit often far from perfectly, so that clinical experiments can be ethically justified. For example, new surgical treatments should be based on a sound understanding of anatomy and physiology. Effectiveness and safety is then established through a hierarchy of clinical trials. On going systematic surveillance is then used to spot rare and serious safety issues. It is not a perfect system and there are many high profile failings. Treatments have a capacity to harm as well as heal, and practitioners can be arrogant or negligent. But a growing regulatory framework exists around practitioners and medical products designed to protect the public.
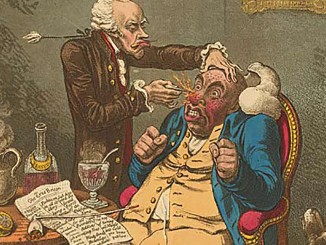
These things are not true of alternative medicine. Indeed, some aspects of alt med are reminiscent of how medicine was before regulation starting pushing medicine into the evidence based world. Beliefs about the safety and efficacy of pseudo-medicines come from two sources: authority and revelation. In this way, alternative medicine beliefs are more akin with religious beliefs than scientific ones.
Homeopaths believe their sugar pills are effective because Hahnemann, the founder, declared a set of rules for universal healing. Being effective for a homeopath is a matter of selecting the right ‘remedy’ based on these rules. If a patient does not get better, it is not because homeopathy is nonsensical, it is because the homeopath did not chose the correct remedy. Safety is not established through long term, systematic monitoring of outcomes, but because homeopaths assert their practice is ‘holistic, natural and works in tune with the body’. Wider aspects of safety, beyond the sugar pill, are not considered. Homeopaths may assert that they have been “effective for 200 years”, but this is a statement of mere authority based on post hoc interpretations of their treatments – usually confusing the natural course of illness, regression to the mean, and selective reporting as effectiveness. Of course, high quality clinical trails fail to demonstrate clear effectiveness.
Acupuncturists also base claims of effectiveness on tradition – a tradition that stretches back meaningfully only a few decades – not thousands of years as claimed. Over the past 50 or 60 years, a lore of knowledge has built up on where mystical meridians lie on the body and how chi gets blocked. Effectiveness is about putting needles into the correct place in the body as described by various authorities. Again, various ad hoc excuses will be deployed if a treatment is not effective. There is indeed a huge body of clinical studies of acupuncture that declare effectiveness. However, systematic reviews show the extend of how misleading this research is. All results published in China are positive – as if researchers knew the result before the experiment. And of those studies, most use very poor controls. Studies that better control for artefacts suggest that acupuncture is nothing more than a theatrical placebo – a distraction therapy at best.
Herbalism has many traditions too. Individualised concoctions of herbs are common, where herbs are selected on the basis of authoritative rules based on pseudo-scientific ideas about how ‘hot’ or ‘cold’ a herb may be. Alternatively, zodiacal aspects might be considered. In all cases, the evidence base is not important. The internal philosophy of prescription are.
If evidence is forthcoming from trials, whether positive or negative, it is not used to inform practice within the pseudo-medical world. Negative evidence is dismissed as irrelevant (we know what works – we do not need ‘Western’ science to tell us) or produced by shadowy shills from pharma companies out to discredit techniques that threaten their profit. If the evidence appears positive, then it is used as propaganda and advertising material. No alternative therapy has ever been abandoned as a result of accumulated evidence. Evidence is a tool – a manipulatable resource to be ignored or seized for ends other than creating informed treatments.
Now, regulation of health care is subject to a number of principles. And the House of Lords, when considering the regulation of alternative medicines, made it quite clear that protecting the public depended on a number of simple questions:
“… we recommend that three important questions should be addressed in the following order . .
(1) does the treatment offer therapeutic benefits greater than placebo?
(2) is the treatment safe?
(3) how does it compare, in medical outcome and cost-effectiveness, with other forms of treatment?
However, this perfectly sensible approach is incompatible with how Alternative Medicine works and thinks, as we have seen. Any regulatory body with a meaningful approach to these questions will demand to see robust, large scale randomised controlled trials to support the case for a therapeutic benefit, before claims can be made. They will want to understand how the safety of the treatments are evaluated and monitored. But this is completely alien thinking to alternative medicine who do not understand such issues in terms of the rational and the scientific. Therefore, the mainstream approach to regulating health practices should be anathema to them.
There are several responses that pseudo-medical practitioners can make to this dilemma: firstly, they can seek alternatives to statutory regulation through voluntary or trade style regulation. We can see such practices occurring through the myriad of ‘professional regulators’ that exist in the alt med world. The government has also dabbled with setting up Ofquack (http://www.ofquack.org.uk) – the Complementary and Natural Healthcare Council. Voluntary regulation is just a fig leaf though, and completely fails to protect the public from the dangers posed by their members as the examples of the Society of Homeopaths and Ofquack show.
But the prize of statutory regulation is too great to ignore as it gives status, trade protection and access to state funds through University’s quackademic courses and referrals from the NHS.
The next approach to get around the evidence dilemma is to weaken the importance of evidence in regulation. The regulator could be asked to regulate a practice despite their being any evidence of it being a real medical therapy. The Health Professions Council shamefully appears to suggest that it is willing to do such a thing because regulation is still ‘in the public interest’. How the public can be protected when people are given a green light to make baseless healthcare claims is just not clear.
But most insidiously, the next tactic is to create a regulatory environment where the very concepts of evidence in medicine are undermined. This strategy is routinely employed by alternative medicine enthusiasts who claim that RCT evidence is not applicable to ‘holistic’ therapies (without ever explaining quite why) or that RCTs are themselves inherently unsuitable and other forms of ‘evidence’ are desirable.
We saw Professor George Lewith try this tactic today in a BBC report into a trial where placebo expectations had significant effects on perceived pain. He said,
It’s another piece of evidence that we get what we expect in life. It completely blows cold randomised clinical trials, which don’t take into account expectation.
This is absurd nonsense. As the blogger Majikthyse says on his blog,
Is not this study a “cold randomised clinical trial” its very self? This from a professor who is employed to run “cold randomised clinical trials”. To claim that one randomised controlled trial (RCT) in a single therapeutic area invalidates the entire discipline of clinical trials is bizarre and not remotely supported by the evidence. But this study simply doesn’t mitigate in the slightest way against RCTs, because it is an RCT. Sorry, but in case Lewith is reading this I have to make it crystal clear.
It looks a lot like bandwagon jumping to me.
Quite.
The new College of Medicine, the quackery promoting organisation that has arisen from the ashes of fraud of Prince Charles Foundation for Integrated Health is also very keen to muddy the water around medical evidence. The College intends to ‘commission a full-scale review on the nature of knowledge for clinical practice”. Given the objectives of the FIH and the people involved, there can be little doubt that this review will help undermine the very concepts of evidence that enable us to make informed choices about treatments and in doing so, let in all forms of quackery through the back door.
So, to answer my question I set in the title: how do we spot bad regulation of alternative medicine. Well, let me suggest the Quackometer rule of thumb on the issue. A basic tenet of regulating quackery: if the quacks are happy with the proposed regulation, then it will not be effective regulation capable of protecting the public from misleading claims, ineffective treatments and dangerous beliefs.
Any regulatory regime that is acceptable to the mode of thinking found in alt med must somehow avoid the obvious issue of answering the most critical question of how we know if the treatment works or not. Ineffective treatments are inherently harmful. Regulating ineffective pseudo-medical treatments gives false choices to patients and disenfranchises them from having appropriate informed consent about what is right form them. Such statutory regulation then becomes simply a matter of providing trade protectionism – state sanctioned statutory cartels of superstitious medical practices.
The regulatory cartels allow the quacks to create monopolies of control over what they do, protect themselves from external regulatory forces, such as Trading Standards, increase their status to that of other real health care providers and compete for the same public funds on an equal footing to meaningful and evidenced treatments.
This week has seen some examples of how alternative practitioners have been trying to influence government to provide favourable regulatory regimes.
As I reported in my last blog post, homeopaths are panicking that the medicines regulator is reconsidering how it gives licenses to homeopathic products, what claims can be made and what form of wording should be allowable on labels.
The MHRA made a serious mistake in 2006 by allowing homeopathic product manufacturers to make claims about effectiveness, not on the basis of evidence, but on the basis of tradition. As you might, guess the homeopaths were overjoyed about that. (It is suspected that Prince Charles was directly involved with lobbying the government to allow this.)
The MHRA are now considering that the labels should make it clear that claims are made on the basis of use “within the homeopathic tradition”. In their panic letter, they urge the MHRA to keep this wording as it “avoids the need to prove the science behind prescribing of remedies and allows us to practise as normal.” It is a damning statement.
The next insight this week comes from the government’s announcement of how it intends to regulate herbalists (and in the future, acupuncturists).
Health Minister, Andrew ‘La La’ Lansley, has not listened to medical profession about the dangers of providing statutory regulation for unproven and nonsensical treatment and has gone along with the herbalists and plumped for a list of “authorised healthcare professionals” that are allowed to prescribed unlicensed herbal products. This has saved the bacon for herbalists, as under new legislation coming in this Spring, only licensed herbal products can be sold to the public directly and unlicensed products require a person with appropriate authorisation to ‘prescribe’.
So, the government has used the platform of statutory regulation to ensure a quack trade survives what would have otherwise been a quick death. The plethora of High Street herbalists that have sprung up over the past decade, making outrageous claims for their dried plant material, will be protected by undermining the whole concept of having registered health professions.
There is no justification to be made here that suggests the public will be protected by this move. Indeed, it is a state sanctioned license to mislead and profit from people’s health concerns. (see Meddling Princes, Medical Regulation and Licenses to Kill)
The report on the consultation from the Department of Health [pdf]suggests that there was a consensus amongst the majority of responders that this was the right move. Of course, the majority of responders were desperate herbalists trying to cling onto their income. I expect that the usual mistake was being made of using that practitioners of alternative medicine are experts in the subject when the reverse is true (for reasons I spell out here: When the Regulator Believes in Fairies, Who Protects the Public?) The real experts in medical care and regulatory matter, the Academy of Royal Medical Colleges, were dismissed as a ‘minority’ voice in the summary – and indeed, views were published from the herbalists that such voices would be protecting their own interests. And again, the mistaken view that a well-trained quack is safe quack won the day when the exact opposite is the case: such people are thoroughly bought into their cults and made impervious to evidence and reason. (See my report on how homeopaths were taught to mislead their clients doctors’ about compleence with treatments for communicable diseases: Can We Trust Homeopaths to Accredit Their Own Training?)
So perfectly sensible legislation, designed to protect the public from herbal products whose safety and effectiveness cannot be demonstrated, has been undermined by the corruption of statutory regulation of medical professionals.
These mistakes are made, in part I am sure, because most people have a very inaccurate view of what alternative medicine is. In short, it is neither alternative nor medicine. Practitioners are members of pseudo-medical cults with beliefs about supernatural forms of medicine that are impervious to reason and evidence. The threat to the public comes rarely from the sugar pills, tiny needles, plant matter or back massage, but from the dangerous beliefs that run counter to well established medicine, their hatred of vaccinations and the way they undermine trust in medical professionals with absurd conspiracy theories and impugned motives.
So, in summary. If the homeopaths, herbalist and chiropractors are in favour of a form of regulation, it is almost certainly designed to protect them and not protect the public. What is required is not proteciton of title and registers, but better prosecution of people who make misleading claims. We already have good legislation under Trading Standards. It is time that these people were given the resources to do their job in this out of control sector.


Andy said:
Nail. Head.
“Nail. Head.”
Yep. And this:
Interesting post. No issues with Homeopathy or Accupuncture, but finding problem with Herbalism (assuming you mean european medical herbalists)
You know probably better than me that research has shown that some herbs work. Infact a large proportion of the modern medical pharmacy is derived from flora, as you also know.
So is the problem you really have with the training of herbalists?
If the standards of training aren’t adequately governed,then this allows the woo in (astrology etc). In my opinion only statutory regulation.
1)weed out the woo merchants (no pun intended)
2)set standards for recognised qualifications that allow entry to register
If minimum standards were to include anatomy, physiology, pathophysiology, pathology and clinical methods this should start to increase their patient safety.
If diagnosis were made from agreed western pathologies, this should further increase safety
If the herbal practitioner doesn’t conform to these standards they can be removed from the register and not allowed to practice as a herbalist (further protecting the public)
There will be some people (misguided or not) who have problems with big pharma. They have the choice of herbal remedies. At the moment they have the choice of buying this off the shelf from many “health” food shops. They make their (un)informed choice of remidy from magazines and newspapers. thinking it’s natural therefore it’s safe.
If they were more informed they might find out there are side effects and cross reactions with other meds. This is again where a registered herbalist should be involved. With the correct training they should know all this, and be able to prescibe the correct herb. If they don’t think their remedies are appropropriate they will then refer back to their GP (maybe limit of competance included in registration requirements)
Sorry for long winded ramble, but was trying to get through rather a lot!
But most herbal treatments don’t work. Read R Barker Baussell’s book or Ernst and Singh’s.
Sure, some herbal preparations have biological effects. They have therapeutic effects and side effects that can be dangerous. Pharmaceuticals have been derived from herbal sources with efforts directed precisely at opening up the gap between these effects.
Herbalism comprises the scrapings at the bottom of the bin. Things that can’t work. Things that don’t work. Things that work but are toxic. If there is a good apple remaining in the barrel a “licensed” herbalist is absolutely not the person who can be relied upon to find it. Nor should he or she be given a state licence to con the public with their fanciful ideas on the off-chance that somewhere among their jars of shrivelled leaves there is something useful hiding away. Drug discovery is the job of systematic scientists not superstitious fools.
As I said below, I believe this this is an issue of medicine versus proto-medicine versus pseudo-medicine.
You should also read this grim document to find out what unfettered woo practitioners do;
http://www.safetyandquality.health.wa.gov.au/docs/mortality_review/inquest_finding/Dingle_Finding.pdf
The only reason this is not a more widespread problem is because few people are so stupid as to avoid real medicine when they have an actual serious illness.
There is no evidence that, left to their own devices, SCAM practitioners have any systematic ability to triage serious illness.
Simon Singh’s sting of homeopaths on the subject of malaria was a good example of their dangerousness.
An observation and a question:
Um-teen decades ago, when science and sense was being applied in the apothecaries, some preparations were found to work. Naturally, one assumes, these were produced in increasing volumes. And so the phamaceutical industries thrived.
Now, back in those days, some preparations were clearly NOT developed in this way – most likely since they were little more than useless.
So my question is: is it now the useless that has become the alternative?
In broad terms, I think the answer is yes.
However, in herbal traditions that have been less explored by systematic methods there are some gems still to find. But Big Pharma has organised projects to search these out.
Big Quacka has no systematic methods to do anything meaningful. Indeed, worse, they have locked themselves into parallel systems of belief which positively undermine any ability to judge efficacy because their systems provide pseudoexplanations for everything. Because they think they can explain all outcomes they have no anomalies or oddities to explore. Scientific medicine, in contrast, focuses effort precisely at those anomalies. A classic example would be the recognition that drugs have very specific structural requirements in order to work. This prompted the question as to why this should be. The answer was the existence of receptor molecules, which implied the existence of “endogenous ligands”, i.e. chemicals intrinsic to the body, for which these receptors are the natural site of action. The search for endogenous ligands then opened up whole new avenues of research for the optimisation of the effects of drugs acting at those sites.
It’s important not to fall into the middle-class trap of lumping all CAM together. Herbalism is not pseudo-medicine, it’s more like proto-medicine. If you were to draw a clade diagram of the evolution of medicine, the mainstream and herbalism diverged relatively recently. Herbalism is the coelacanth to medicine’s homo sapiens: an evolutionary backwater which stopped evolving and is now mainly to be seen preserved in formaldehyde. Traditional medicine practitioners are, for the most part, conducting historical re-enactments. Herbs have real, provable and in many cases provably effective pharmacologically active compounds, it’s just that by now we have worked out a better way of delivering them and a more scientific way of prescribing them.
Homeopathy, by contrast, is a completely separate tree positioned out into left field somewhere. It has no obvious connection with the evolution of modern medicine beyond the occasional coincidence (cinchona bark and Edward Jenner being the obvious examples). It has not evolved because it has no mechanism for self-correction, anything believed once is believed in perpetuity, however absurd it may be. Its function as a belief system not as a system of medicine is obvious from a study of the inconsistencies between the pronouncements of its various prominent advocates.
I am not sure what is ‘middle class’ about lumping heralism in with other pseudo-medicines. In fact, I would disagree with you in saying that herbalism should be seen as a proto-medicine. I think it is this view of herbalism that allows it an easier route into statutory regulation and needs to be challenged and examined very closely.
Herbalism, though does indeed have many ‘traditions’. The proto-medicine part, I would say corresponds to those few herbs that will indeed be licensed under the new scheme and will be available in Boots. These concoctions are used with a type of mainstream diagnosis and application – there is a one-to-one correspondence between a condition and a herb and that herb will have specific effects.
But the statutory regulation of herbalism will be covering those plant materials where there may well be no analogue with mainstream diagnosis and prescription.
The English Herbalism tradition is heavily influenced by Culpepper who took an astrological view of the illnesses and plants and saw correspondences between zodiacal characteristics and various plants. On our High Streets we see Ayurvedic and Chinese herbalism which are influenced by superstitious views of anatomy, spirituality and health. In all, there is a strong influence of the magical and shamanic in approaches.
Some ‘modern’ herbalists take on the popular discourse of alternative medicine and use a functional approach – e.g. detox. As such, I see little reason to differentiate herbalism from other forms of pseudomedical practices. It is likely that much of the plants used are essentially inert (or produce arbitrary effects, such as nausea). The ‘theatrical’ component of herbalism is all that differs from the sugar pills of homeopaths, the pins of acupuncturists and the bone cracking of chiropractors.
Herbalism may have been a “proto-medicine” a couple of hundred years ago, but medicine has moved on since then.
Guy, I can see the appeal of that image but there is an essential difference. At any given time in evolution you could take a contemporaneous cross-section of the existing lifeforms and you would say that each seems marvellously adapted to its environment. It is only with the passage of “deep time” that we see lifeforms shifting and can then impose a narrative that implies maladaptation of the previous forms.
With herbalism vs medicine, the prior form is clearly maladapted, but it has failed to die out.
The coelacanth is a success having survived with minimal change over millions of years. Herbalism is a failure having survived with minimal change for thousands of years.
Maybe I’m just taking your analogy too seriously, but I think these are interesting points.
Surviving without change is a defining characteristic of sCAM. After all, if your practices aren’t based on evidence in the first place, why change them if conflicting evidence appears?
The problem is that they get away with presenting this as a strength.
Could I suggest that a small flotilla of black ducklings makes its way here;
http://www.cogitamus.co.uk/?p=290
They may not publish your comments, but they deserve to hear that many of us do not think theirs was a job well done.
Does that mean the homeopaths have retained their rights and continue in practice as normal?
Maybe only a battle lost?
I got this from Blue Woads twitter and it has appeared on other sites.
How can this be allowed to be published about professor Ernst, surely this is inaccurate?
http://smperle.blogspot.com/2010/12/self-importance-of-being-ernst.html
There is a principle which is a bar against all information, which is proof against all argument, and which cannot fail to keep man in everlasting ignorance. That principle is condemnation without investigation. William Paley (1743-1805)
Indeed.
Only problem, Kaviraj, is that we have investigated homeopathy. And now we condemn it.
I had very little opinion of homeopathy until I investigated it. It was the claims and activities homeopaths themselves that prompted me to take an interest. Now, a decade later I am quite content to condemn homeopathy and condemn homeopaths for practising it despite its internal inconsistencies and illogic.
Anyway, thanks for popping by. It’s been interesting to see how quiet it’s gone at the site of your buddy Benneth recently
Kaviraj – As BSM says, this site is a very comprehensive investigation into homeopathy and homeopaths. And I condemn many of its practices and beliefs because of that investigation.
But please keep to the topic.
Google Shuts Down Quackbuster Discussion Group…
http://www.bolenreport.com
Keep to the topic, Kaviraj. Off topic comments may well be removed.
Not sure what this group is/was or what or who bolenreport is, but it does not appear pertinent to the issues.